
Here is the income bracket you have to be in to afford a home in Toronto right now
Toronto's real estate market has for months been characterized by the total opposite of what has historically defined it, with unusually high inventory levels, desperate sellers, easier price negotiations and, most importantly, lower mortgage rates.
These factors have combined to finally make homes in the region a bit more affordable, even if asking prices have not tumbled as far as residents had hoped.
Even month-over-month, the amount you need to cover a mortgage and other costs on the typical home is dropping, not just in the GTA but across the country.
Toronto has so many condos up for sale that it's becoming a buyer's markethttps://t.co/WIu1RQWzPv
— blogTO (@blogTO) October 10, 2024
The latest insights from Ratehub.ca, which assesses the salary required to afford a house or condo in major Canadian hubs each month, shows this figure decreasing by thousands in some cities between September and October 2024.
In Toronto, being the second most expensive place for real estate in the country, these declines have been among the most significant.
"Interest rates continued to drop month-over-month, which means improved affordability again this month," the firm wrote in a release on Wednesday. "Twelve out of 13 cities that we studied saw a drop in income required to purchase a home."
Of these cities, Vancouver saw the most substantial change in the income needed for a home as far as dollar amount, while Hamilton saw the biggest reduction, percentage-wise.
In the B.C. capital, the mean home price fell by $7,700 (to a still-ridiculous $1,172,000) over one month, pushing the annual earnings necessary to float such a purchase down by $4,540 (now $214,460) at current mortgage and stress test rates, which were lower in October than in September.
In Toronto, the average cost of a place of one's own plummeted by $7,700 (to a whopping $1,060,200), meaning a household now needs to rake in $4,380 less per year (a total of $195,420) to fund one.
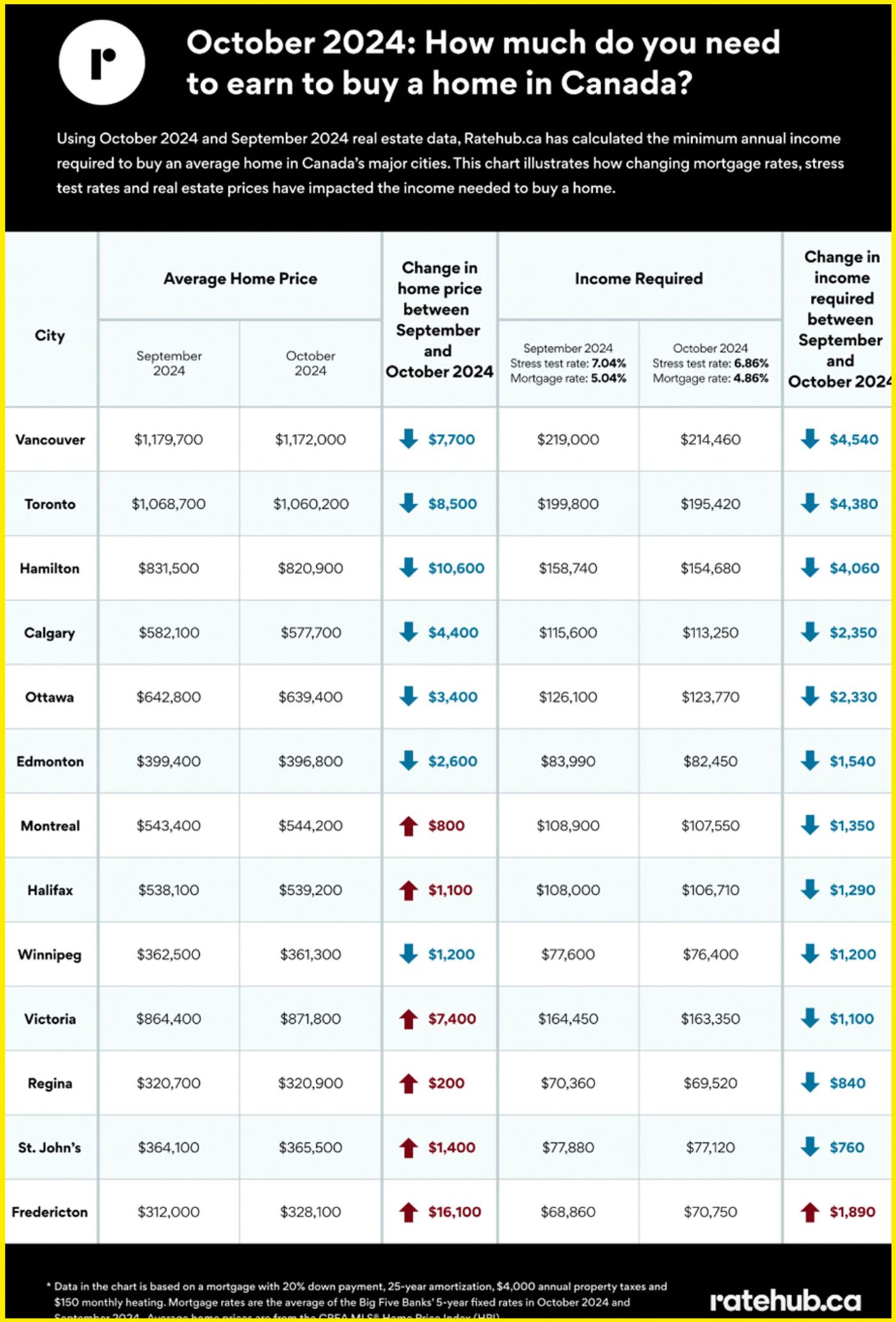
How the salary needed to pay for the standard home in various metropolitan areas in Canada has changed in the last two months. Chart from Ratehub.ca
If you want something remotely affordable within Canada's tragically overpriced bounds, your only hope appears to be somewhere like Regina, where the cost of the typical listing and the salary needed to pay for it may have fallen by only $200 and $840, respectively, in the last two months, but where a home is only around $320,900 (which can be paid off at current rates with $69,520 a year).
Fredericton, St. John's, and Winnipeg are also fairly cheap, with homes priced between $328,100 and $365,500, warranting earnings of $70,750 to $76,400 annually.
Ratehub offers some hope by pointing to the fact that interest rates are due to trend even lower in the near future, which should help offset a shift in demand that many experts say is already starting.
IMaggs/Shutterstock
Latest Videos
Latest Videos
Join the conversation Load comments







