
Here's what Toronto's new direct train to Muskoka will look like
The new rail line that will connect Toronto directly to cottage country locales such as Muskoka, as well as even further north, has just crossed another major milestone on its way to completion.
And in announcing that milestone, the provincial government has released some new renderings of what the shiny new trains will look like.
Ontario Minister of Transportation Prabmeet Sarkaria shared on Friday that the team tasked with creating the platforms and shelters along the new-and-improved Northlander line has now been selected, meaning work on these crucial assets can start imminently.

Rendering from the Province of Ontario's release on December 6.
Old stops along the defunct train's route — in North Bay, Temagami, Temiskaming Shores, Englehart, Kirkland Lake, Matheson and Cochrane — will be renovated and outfitted to prepare for the first passengers the line has had in well over a decade. The new hubs will benefit from improved accessibility, lighting, signage and more.
Meanwhile, the sleek, state-of-the-art new train carriages from Siemens Mobility Limited will offer galley-style food services and Wi-Fi and will come equipped with wheelchair lifts, mobility aid storage spaces and fully accessible washrooms.

Rendering from the Province of Ontario's release on December 6.
Premier Doug Ford has been promising to bring back the Northlander Passenger Train for a few years now, saying that its discontinuation in 2012 had "cut people and economies in Northeastern Ontario off from the rest of the province."
Though limited bus service has operated in lieu of the passenger rail, the initial business case to bring back the Northlander stated that "some residents in Northern Ontario have identified challenges in using the existing bus service," as it "operates within mixed traffic on the road network, which exposes the service to disruptions on the road network and decreases travel time reliability."
It also pointed out how inclement weather can lead to highway closures due to particularly poor road conditions unique to the north of the province and accidents that happen as a result. With limited detour options, the four daily bus trips in each direction between Toronto and North Bay can be compromised. Passengers to and from destinations further north also have to transfer in North Bay or Sudbury.
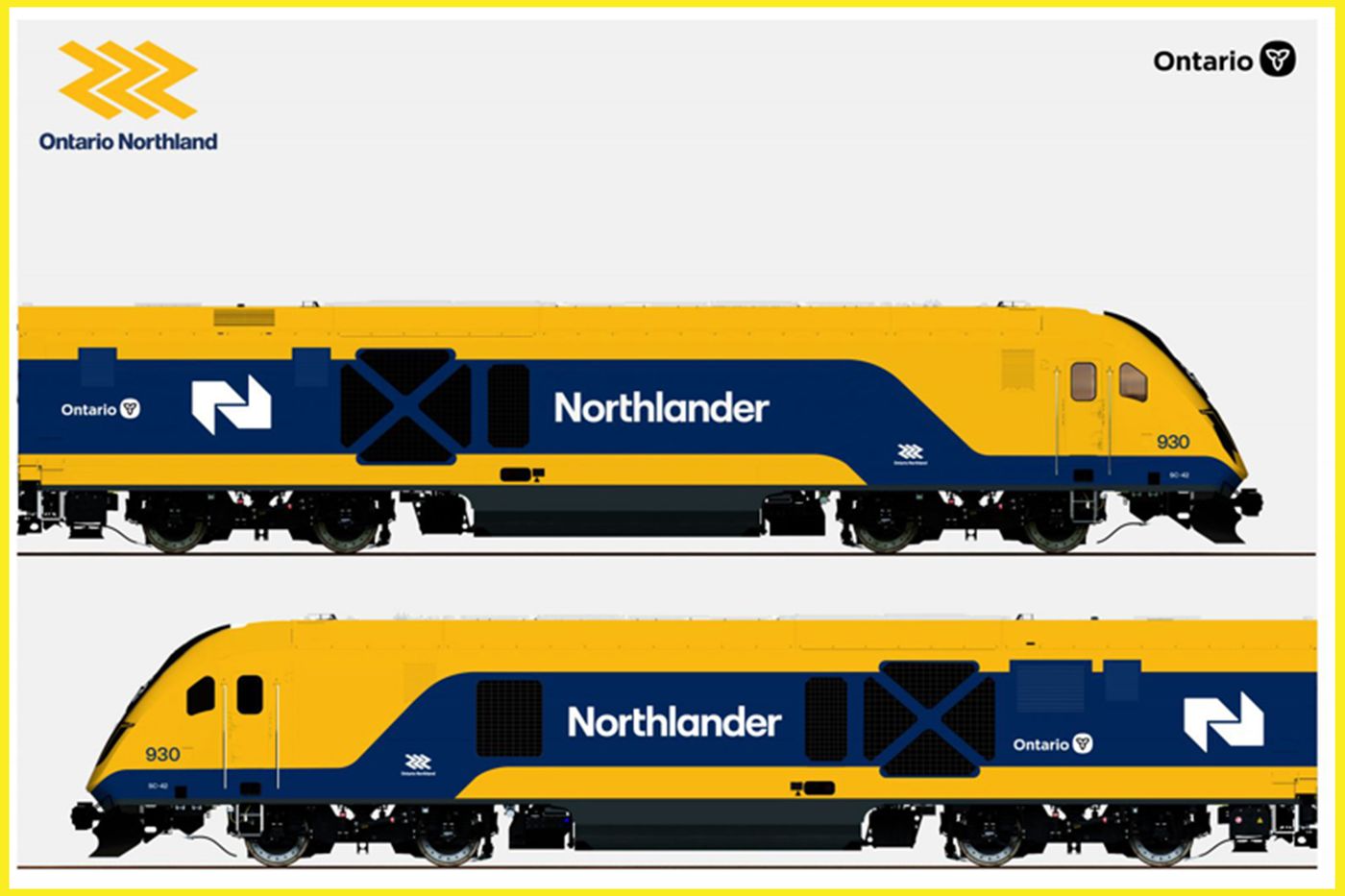
Rendering from the Province of Ontario's release on December 6.
Funds were earmarked in Ontario's 2024 budget specifically for the return of the transit option, which will service 16 stations between Toronto Union and Timmins from four to seven days a week, contingent upon seasonal demand.
As one local representative, Timmins MPP George Pirie, celebrated in a release on the latest news, "Northern Ontario has always been a major contributor to our provincial economy, with potential for further growth in the years to come. By fulfilling our promise and bringing back the Northlander, our government is connecting the north to new economic opportunities and enabling improved access to services."
New direct train route from Toronto to Muskoka now a step closer to reality https://t.co/W5OLVupiVf
— blogTO (@blogTO) June 3, 2024
Construction giant EllisDon has been awarded the contract to begin work on the passenger stops north of North Bay, while three separate companies (Enseicom Inc., Remcan Ltd. and X-Rail) were chosen to build and install the pre-fab shelters passengers will wait in, to perform refurbishments to the existing tracks, and to complete warning signal upgrades.
Still yet to be awarded is the contract for the line's northern terminus, the forthcoming Timmins-Porcupine station.
Alessandro Cancian/Shutterstock
Latest Videos
Latest Videos
Join the conversation Load comments







