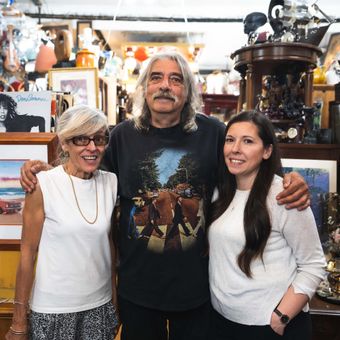
TreaJah Isle is Toronto's world famous reggae record and convenience store
Hot Spots
Posted on July 19, 2021
You can't talk about the history of Toronto's Little Jamaica without mentioning TreaJah Isle. A cornerstone in the community for three decades, this reggae record store has hosted legendary musicians, all while staying true to the neighbourhood it's in.
Produced, filmed and edited by Aaron Navarro.
Your inspiration for places to eat and things to do in Toronto. Plus news, events and more. New videos posted daily. View all videos